
Equine Health Library
Senior Horse
Health Concerns
Musculoskeletal | Endocrine
Musculoskeletal
Musculoskeletal
Muscle and joint problems are one of the most common disorders in senior horses and are often compounded by conformation faults, degenerative conditions or underlying endocrine diseases.
Muscles, Joints and Lameness
Did you ever wonder why old horses often look swaybacked? As horses age, they lose muscle mass – both as part of the aging process and due to reduced exercise and conditioning. The ligaments that support the back also weaken, making the withers appear more prominent. Underlying, untreated endocrine diseases such as PPID can accentuate this muscle loss and swaybacked appearance.
You also may notice dropping of the fetlocks in your old horse, especially in the hind legs. This may be a result of degeneration of the suspensory ligaments. It’s more common in certain breeds and can be made worse by late-stage pregnancy in older broodmares.
As always, if your older horse is starting to have a more difficult time just getting around, call your veterinarian for a full workup.
Degenerative joint disease
As horses age, so do their joints and all of the structures associated within the joint, especially the cartilage. Cartilage damage is the hallmark of degenerative joint disease (DJD) in the senior equine.
Joint cartilage can become damaged due to overuse, a traumatic joint injury, infection or normal, age-related wear and tear. Cartilage has a very limited ability to regenerate and heal, which is why DJD is not reversible and usually progressive. However, through the use of modern medicine, DJD can be diagnosed and managed so that many senior horses can live a more comfortable, longer life.
DJD can show up as varying degrees of lameness. A thorough physical examination by a veterinarian – including a lameness evaluation – will help determine which joint or joints are affected. This exam might include radiographs (X-rays) and/or an ultrasound. These tests will help determine the severity of the DJD and the proper course of treatment and future management.
Treatment first focuses on addressing the most likely cause (e.g., improper shoeing, poor hoof/pastern axis) and then managing pain and preventing progression of joint damage.
Prescribed Treatment Options
- Rest
- Physical therapy
- Corticosteroids (either systemic or intra-articular)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as phenylbutazone or Banamine® (flunixin meglumine paste)
- Chondroprotective agents such as sodium hyaluronate (HA), polysulfated gycosaminoglycans or other nutraceuticals
- Orthobiologics such as platelet rich plasma, stem cell therapy, interleukin-1 antagonist receptor protein, autologous conditioned serum, alpha-2 macroglobulin, and amnion extract.
With proper care and treatment, senior horses with DJD can remain pasture sound or even rideable well into their 20s and 30s.
Important Safety Information
For Oral Use in Horses Only. Not for use in horses intended for human consumption. Do not use in horses showing hypersensitivity to flunixin meglumine. The effect of BANAMINE Paste on pregnancy has not been determined. Concomitant use of Banamine with other anti-inflammatory drugs such as NSAIDs and corticosteroids should be avoided or closely monitored. For complete information on Banamine® Paste, see accompanying product package insert.
Laminitis
Perhaps there is no diagnosis more dreaded by horse owners than one of laminitis. An inflammation of the laminae of the hoof wall, laminitis is a very painful condition that can have varying degrees of severity. The onset of signs can be slow and subtle or acute.
In the most severe cases, the laminae are so inflamed that the third phalanx (aka the coffin bone) that is supported by these structures rotates and can penetrate the bottom of the sole. These horses experience extreme pain and spend the majority of their time lying down. Due to poor prognosis and poor quality of life, these horses are often euthanized.
Other cases of laminitis are not as severe and can be treated and managed with proper diet and corrective shoeing.
Signs of acute laminitis
- Lameness, especially when a horse is turning in circles; shifting lameness when standing.
- Heat in the feet and increased digital pulses in the arteries supplying blood to the feet.
- Pain in the toe area when hoof testers are used.
- Reluctant or hesitant gait.
- Standing with the front feet stretched out in front to alleviate pressure on the toes and the hind feet positioned underneath the horse to support the weight.
- Puffy coronary bands with possible clefting.
Signs of chronic laminitis
- Rings in the hoof wall that become wider as they are followed from toe to heel.
- Bruised soles.
- Widened white line with blood pockets and/or abscesses.
- Dropped soles or flat feet.
- Dished hooves, resulting from the heels growing faster than the rest of the hoof.
Researchers are still working to discover how and why laminitis happens, but we do know several risk factors, including:
- Increase in carbohydrates (horse gets into the feed bin or too much time on new, green grass or clover).
- Mechanical overload (a horse with an injury such as a fracture will bear more weight on the uninjured leg, thus predisposing it to laminitis).
- Certain disease conditions such as PPID.
- Severe, systemic bacterial illnesses (e.g., septic metritis in a postpartum mare or a horse with Potomac Horse Fever diarrhea) that result in release of toxins into the blood stream.
If you are concerned about laminitis, talk with your veterinarian right away as early intervention is the best chance for a positive outcome. Therapy for laminitis can vary, but includes pain medication, anti-inflammatory drugs and proper foot support. Icing the affected feet is a very effective therapy during acute stages of laminitis. Chronic cases of laminitis require teamwork between your veterinarian and farrier to provide proper trimming and shoeing as indicated by radiographs and clinical signs.
Maintaining a proper body condition score and having routine veterinary examinations play an integral role in helping to prevent laminitis.
Endocrine
Endocrine
PPID
If you’ve seen an old horse with a long, curly haircoat that never seems to shed, you have probably seen a horse with pituitary pars intermedia dysfunction. PPID is one of the most common hormonal disorders in horses.
This disorder is thought to be the result of age-related oxidative stress that leads to degeneration of neurons that normally inhibit the pars intermedia portion of the pituitary gland. With this degeneration of neurons, an environment occurs where a tumor can develop within the pituitary gland. PPID is the result of a tumor (pituitary adenoma) in the pituitary gland which causes the adrenal glands near the kidneys to produce too much of the stress hormone, cortisol.
Symptoms of PPID include excessively long haircoat, delayed shedding, sway-backed appearance due to muscle wasting, excessive drinking and urination, intermittent and spontaneous sweating, immune suppression, and increased incidence of laminitis.
Your veterinarian will diagnose PPID based on physical examination, clinical signs and endocrine testing. While there is not a cure for PPID, affected horses can generally be managed successfully with administration of the medication, pergolide.
It’s important not to confuse PPID with Equine Metabolic Syndrome, another endocrine condition that can affect senior horses. Although clinical signs may overlap, bloodwork is needed to differentiate these conditions and determine a treatment/maintenance plan.
Action Item
Perform endocrine testing in horses experiencing unexplained bouts of laminitis, changes in haircoat, increased drinking and urination, excessive sweating, increased appetite, muscle loss (especially along the topline), a potbellied appearance, and/or abnormal fat deposits.

Pony with PPID. Note long, shaggy hair coat.
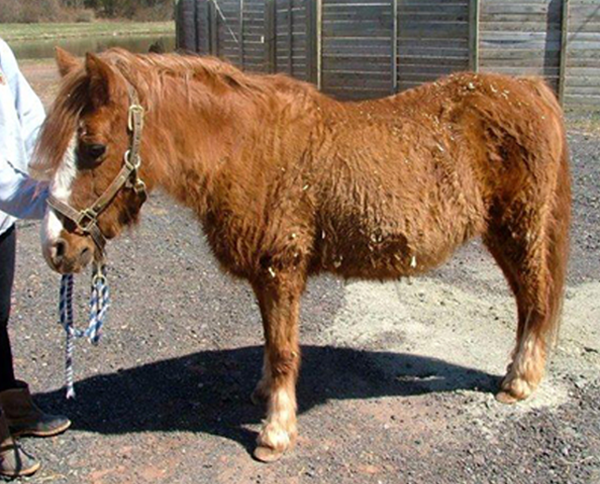
Another pony with PPID. Note the long hair coat that failed to shed out during the spring. Other signs of PPID include pendulous abdomen due to loss of tone of body musculature, increased water consumption and urination, lethargic attitude, and patchy sweating.
Other Concerns
Heart
Just like people, aging horses frequently experience an increased incidence of heart disease. These diseases are often accompanied by cardiac murmurs of varying intensity.
Your veterinarian may first detect a cardiac murmur during a physical examination and can further diagnose heart disease through an EKG or echocardiography. Your senior horse could have leaky or compromised heart valves (such as mitral and aortic valvular insufficiency), which can increase the workload of the heart and make it harder for your horse to tolerate exercise. Talk to your veterinarian if you’re noticing that your horse becomes easily fatigued or out of breath sooner than before.
Eyes
Since many senior horses can have problems with their eyes, it’s important to include an annual ophthalmic exam in your horse’s physical. That way, your veterinarian can detect progressive changes before they compromise your horse’s vision. The most common eye abnormalities include cataracts, vitreous degeneration and senile retinopathy.
If your horse has battled recurrent bouts of uveitis (moon blindness) throughout his life, he may also have some of these changes. Luckily, active inflammatory conditions can often be controlled with a variety of topical and systemic therapies.
